“It’s been a rollercoaster journey – from not knowing what vitiligo was, to trying every medicine I could find and now embracing and accepting that I look different.”1
There are no approved treatments for vitiligo in Europe. In fact, 65% of European patients have been told their condition is completely untreatable.2 This means the only positive outcome many patients can work towards is acceptance instead of relief.
How to diagnose vitiligo
Diagnosing vitiligo correctly is key to helping patients better understand their condition and for HCPs to manage the disease. 45% of all patients in Europe have had their condition misdiagnosed.2
Vitiligo diagnoses are based on:
- Physical examination (with or without Wood’s lamp)4,5
- Clinical history4
- Laboratory tests (e.g. thyroid function, autoantibodies)4,6
- Biopsy of lesional and non-lesional skin4
Progressive disease is marked by:
- Inflammatory, trichrome, and confetti-like lesions7
- Koebner phenomenon — new vitiligo lesions appearing in areas of trauma7,8
What is the goal of vitiligo treatment?
Goal of vitiligo treatment
The goal of vitiligo therapy is:
- 1) Halt disease progression9
- 2) Promote repigmentation9-11
- 3) Prevent relapse9
Lesional skin repigmentation is a complex process which can take months to achieve.
Right image adapted with permission from John Wiley & Sons, Inc. Gan EY, et al. Pigment Cell Melanoma Res. 2017;30(1):28-40. Copyright© 2017.
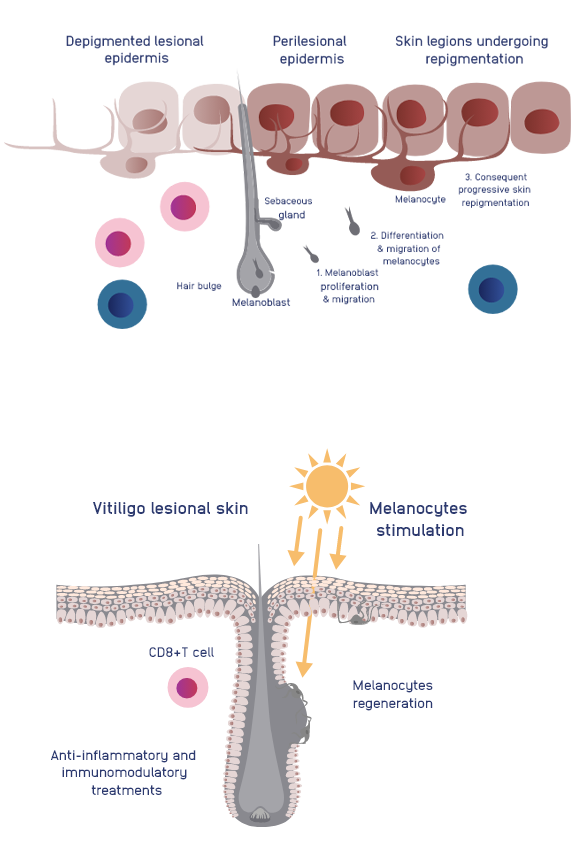
Right image adapted with permission from John Wiley & Sons, Inc. Gan EY, et al. Pigment Cell Melanoma Res. 2017;30(1):28-40. Copyright© 2017.
Repigmentation – a slow and gradual process
Repigmentation – a slow and gradual process
Lesional skin repigmentation is a slow process which can take months to achieve.
It’s thought to occur via the:
- Migration of melanocytes from perilesional skin12
- And/or Migration of melanoblasts from stem cell reservoirs, such as hair follicles and sebaceous glands12
Areas with low, or no, hair follicle density such as mucosal or semimucosal surfaces, lips, wrists and genitals are resistant to repigmentation.12
Limitations of current disease management in Europe
There are no approved vitiligo treatments currently available in Europe.13
European Dermatology Forum Treatment Algorithm14
| Segmental Vitiligo or Non-Segmental Vitiligo Affecting <2-3% BSA | Non-Segmental Vitiligo | |
|---|---|---|
| 1L | Local corticosteroids or calcineurin inhibitors | Stabilization with NB-UVB phototherapy in combination with systemic/topical therapies with or without localised UVB |
| 2L | Localised NB-UVB phototherapy | Systemic steroid or immunosuppressants |
| 3L | Surgery | Surgery |
| 4L | Depigmentation |
Segmental Vitiligo or Non-Segmental Vitiligo Affecting <2-3% BSA
- 1LLocal corticosteroids or calcineurin inhibitors
- 2LLocalized NB-UVB phototherapy
- 3LSurgery
- 4L
Non-Segmental Vitiligo
- 1LStabilization with NB-UVB phototherapy combination with systemic/topical therapies with or without localised UVB
- 2LSystemic steroid or immunosuppressants
- 3LSurgery
- 4LDepigmentation
Treatment recommendations vary across EU countries*
| UK | France | Italy | Germany | Spain | |
|---|---|---|---|---|---|
| British Association of Dermatologists Guidelines (2021)6 | European Dermatology Forum Guidelines (2013)14* | Italian Society of Dermatology Guidelines (2011)15 | German Vitiligo Working Group Recommendations (2021)16 | Consensus Document on Phototherapy (2005)17 | |
| 1L | TCS once daily or TCI (tacrolimus 0.1% bid) or intermittent regimen TCS topical tacrolimus*† | TCI or TCS, NB-UVB | CS (betamethasone 0.1-0.2% or clobetasol 0.05%)* | TCI or TCS, and/or phototherapy | No official treatment guidelines; scientific consensus for the use of phototherapy |
| 2L | NB-UVB ± TCS or TCI For rapidly progressive, consider oral betamethasone ± NB-UVB | NB-UVB 311nm (for patches <20% BSA), UVA + TCS | In limited vitiligo
| ||
| 3L | Excimer laser + TCI for localised vitiligo Surgery for stable SV/NSV on hands/feet | Surgery (for patients with stable disease >1 year and without Koebner phenomenon) | PUVA 320-400nm (for patches >20% BSA) | ||
| 4L | Depigmentation for extensive vitiligo on visible sites | Depigmentation | Surgery† depigmentation (for patches >50% BSA) |
| UK | |
|---|---|
| British Association of Dermatologists Guidelines (2021) | |
| 1L | TCS once daily or TCI (tacrolimus 0.1% bid) or intermittent regimen TCS topical tacrolimus |
| 2L | NB-UVB ± TCS or TCI For rapidly progressive, consider oral betamethasone ± NB-UVB |
| 3L | Excimer laser + TCI for localized vitiligo Surgery for stable SV/NSV on hands/feet Depigmentation for extensive vitiligo on visible sites |
| 4L | |
| France | |
|---|---|
| European Dermatology Forum Guidelines (2016-2020) | |
| 1L | TCI or TCS, NB-UVB |
| 2L | |
| 3L | Surgery (for patients with stable disease >1 year and without Koebner phenomenon) |
| 4L | |
| Italy | |
|---|---|
| Italian Society of Dermatology Guidelines (2013) | |
| 1L | CS (betamethasone 0.1-0.2% or clobetasol 0.05%)* |
| 2L | NB-UVB 311nm (for patches >20% BSA), UVA + TCS |
| 3L | PUVA 320-400nm ( for patches >20% BSA) |
| 4L | Surgery depigmentation (for patches >50% BSA) |
| Germany | |
|---|---|
| German Vitiligo Working Group Recommendations (2011) | |
| 1L | Cosmetics (e.g. Makeup, sunscreen), TCI or TCS, and/or phototherapy |
| 2L | Treatment with topical cortico-steroids is the standard of care for all forms of Vitiligo with an affection of <3% of the body surface area (limited affection*). Treatment prioritisation by lines of therapy not included but recommended to follow 2013 European Dermatology Forum Guidelines |
| 3L | |
| 4L | |
| Spain | |
|---|---|
| Consensus Document on Phototherapy (2005) | |
| 1L | PUVA 320-400 nm NB-UVB 311 nm |
| 2L | No official guidelines but there is a scientific consensus for the use of phototherapy |
| 3L | |
| 4L | |
BSA, body surface area; CS, corticosteroids; NB-UVB/A, narrow-band UVB/A radiation; NSV, non-segmented vitiligo; PUVA, photochemotherapy with psoralen plus UVA radiation; SV, segmented vitiligo; TCI, topical calcineurin inhibitors; TCS, topical corticosteroids.
*Recommendations for therapy vary between NSV and SV.
†For areas with thinner skin. ‡For non-segmental vitiligo; all other treatments are for both vitiligo classifications.
Current treatments are known to have limited success in their outcomes and can result in:
- Low quality of repigmentation18,19
- Short duration of response20,21
- Uneven response in different body regions22,23
- Low treatment compliance24,25
- Kirpal’s story: What makes you different makes you beautiful. Published Winter 2020. Accessed August 2022. https://www.changingfaces.org.uk/story/kirpals-story-what-makes-you-different-makes-you-beautiful/
- Bibeau K, Harris J, et al. Diagnosis and Management of Vitiligo From the Perspectives of Patients and Healthcare Professionals: Findings From the Global VALIANT Study. Presented at: Maui Derm for Dermatologists; January 24, 2022; Grand Wailea, Maui, HI.
- Bibeau K, Hamzavi I, et al. Mental Health and Psychosocial Burden Among Patients Living With Vitiligo: Findings From the Global VALIANT Study. Presented at: Maui Derm for Dermatologists; January 24, 2022; Grand Wailea, Maui, HI.
- Drake LA, Dinehart SM, et al. Guidelines of Care for Vitiligo. American Academy of Dermatology. J Am Acad Dermatol. 1996;35(4):620-626.
- Gawkrodger DJ, Ormerod AD, et al. Guideline for the Diagnosis and Management of Vitiligo. Br J Dermatol. 2008;159(5):1051-1076.
- Eleftheriadou V, Atkar R, et al. British Association of Dermatologists Guidelines for the Management of People With Vitiligo. Br J Dermatol. 2022;186(1):18-29.
- Bergqvist C, Ezzedine K. Vitiligo: Focus on Pathogenesis and its Therapeutic Implications. J Dermatol. 2021;48(3):252-270.
- Njoo MD, Das PK, et al. Association of the Köbner Phenomenon With Disease Activity and Therapeutic Responsiveness in Vitiligo Vulgaris. Arch Dermatol. 1999;135(4):407-413.
- Migayron L, Boniface K, et al. Vitiligo, From Physiopathology to Emerging Treatments: A Review. Dermatol Ther. 2020;10(6):1185-1198.
- Gan EY, Eleftheriadou V, et al. Repigmentation in Vitiligo: Position Paper of the Vitiligo Global Issues Consensus Conference. Pigment Cell Melanoma Res. 2017;30(1):28-40.
- Rosmarin D, Pandya AG, et al. Ruxolitinib Cream for Treatment of Vitiligo: A Randomised, Controlled, Phase 2 Trial. Lancet. 2020;396(10244):110-120.
- Birlea SA, Goldstein NB, Norris DA. Repigmentation Through Melanocyte Regeneration in Vitiligo. Dermatol Clin. 2017;35(2):205-218.
- Incyte. Dermatology. Accessed October 2022. https://incyte.com/dermatology.
- Taieb A, Alomar A, et al. Guidelines for the Management of Vitiligo: The European Dermatology Forum Consensus. Br J Dermatol. 2013;168(1):5-19.
- SIDeMaST. Accessed August 2022. http://www.sidemast.org/download/sidemast_20140609163719.pdf
- Böhm M. Diagnostik und Therapie der Vitiligo. Published online April 23, 2021. Accessed August 2022. https://www.awmf.org/uploads/tx_szleitlinien/013-093l_S1_Diagnostik-Therapie-Vitiligo_2021-04.pdf
- Carrascosa JM, Gardeazábal J et al. Consensus Document on Phototherapy: PUVA Therapy and Narrow-Band UVB Therapy. Actas Dermosifiliogr. 2005;96(10):635-658.
- Kwok YKC, Anstey AV, et al. Psoralen Photochemotherapy (PUVA) is Only Moderately Effective in Widespread Vitiligo: A 10-Year Retrospective Study. Clin Exp Dermatol. 2002;27(2):104-110.
- Yones SS, Palmer RA, et al. Randomized double-blind trial of treatment of vitiligo: efficacy of psoralen-UV-A therapy vs Narrowband-UV-B therapy. Arch Dermatol. 2007;143(5):578-584.
- Boone B, Ongenae K, et al. Topical Pimecrolimus in the Treatment of Vitiligo. Eur J Dermatol EJD. 2007;17(1):55-61.
- Kumaran M, Kaur I, et al. Effect of Topical Calcipotriol, Betamethasone Dipropionate and Their Combination in the Treatment of Localized Vitiligo. J Eur Acad Dermatol Venereol. 2006;20(3):269-273.
- Doghaim NN, Gheida SF, et al. Combination of Fractional Carbon Dioxide Laser With Narrow Band Ultraviolet B to Induce Repigmentation in Stable Vitiligo: A Comparative Study. J Cosmet Dermatol. 2019;18(1):142-149.
- Stinco G, Trevisan G, Buligan C, et al. Narrow Band-Ultraviolet B Versus Clobetasol Propionate Foam in the Treatment of Vitiligo: A Retrospective Study. Dermatol Ther. 2013;3(1):95-105.
- Abraham S, Raghavan P. Myths and Facts About Vitiligo: An Epidemiological Study. Indian J Pharm Sci. 2015;77(1):8-13.
- Alsubeeh NA, Alsharafi AA, et al. Treatment Adherence Among Patients with Five Dermatological Diseases and Four Treatment Types -A Cross-Sectional Study. Patient Prefer Adherence. 2019;13:2029-2038.