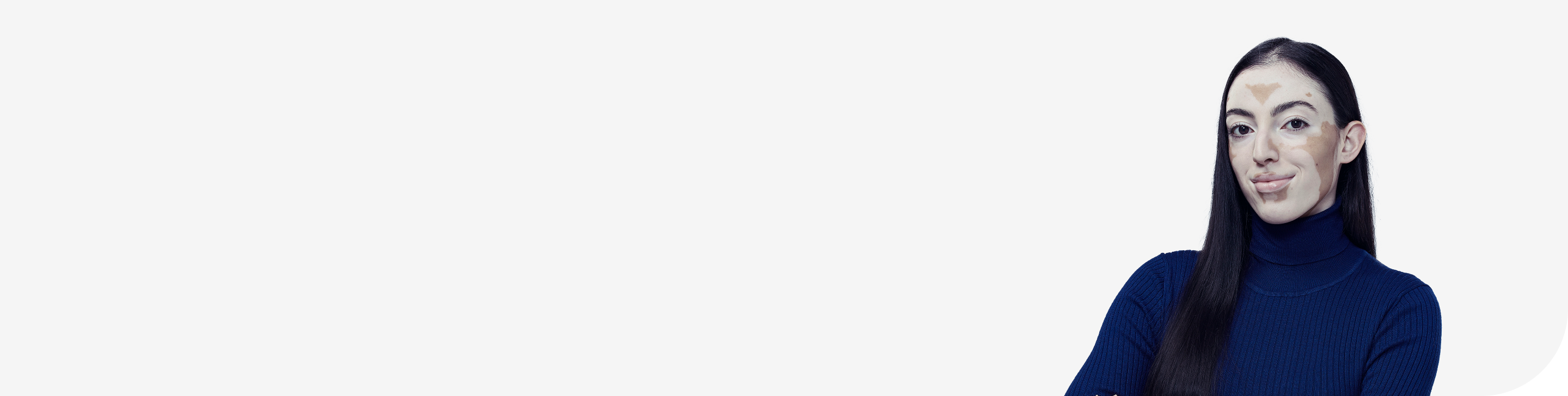
NOW YOU CAN OFFER AN EFFECTIVE CREAM THAT CAN BE APPLIED TO SENSITIVE AREAS AND WORN UNDERNEATH MAKEUP*1
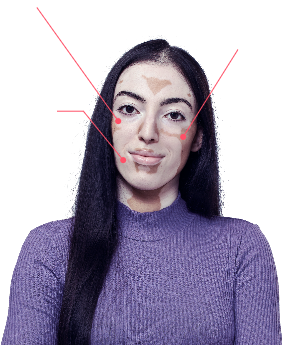
SENSITIVE AREAS44
Opzelura can be used on sensitive areas around the eyes, lips and external genitals†
NON-GREASY CREAM46,47
Opzelura is an easy-to-apply, non-greasy, topical cream

MAKEUP AND SUNSCREEN1,45
Opzelura may be used alongside makeup and sunscreen. At least 2 hours must be observed between the application of Opzelura and any makeup or sunscreen*
* Other topical medicinal products, sunscreen or emollients may be applied with a minimum of 2 hours after the application of Opzelura;† Opzelura should not be applied to the lips to avoid its ingestion. It is not for ophthalmic, oral, or intravaginal use, but may be used on the surrounding areas.
BSA, body surface area.
APPLY IN A THIN LAYER
TWICE DAILY TO AFFECTED AREAS OF UP TO
APPLY IN A THIN LAYER
- 1. Opzelura (ruxolitinib) Summary of Product Characteristics. Incyte Biosciences International Sarl. May 2023.
- 2. Bergqvist C, Ezzedine K. Vitiligo: A focus on pathogenesis and its therapeutic implications. J Dermatol. 2021;48(3):252–270.
- 3. Bergqvist C, Ezzedine K. Vitiligo: A Review. Dermatol Basel Switz. 2020;236(6):571–592.
- 4. Chen X, Guo W, Chang Y, et al. Oxidative stress-induced IL-15 trans-presentation in keratinocytes contributes to CD8+ T cells activation via JAK-STAT pathway in vitiligo. Free Radic Biol Med. 2019;139:80–91.
- 5. Richard MA, Paul C, Nijsten T, et al. Prevalence of most common skin diseases in Europe: a population based study. J Eur Acad Dermatol Venereol JEADV. 2022;36(7):1088–1096.
- 6. Mohr N, Petersen J, Kirsten N, et al. Epidemiology of Vitiligo - A Dual Population-Based Approach. Clin Epidemiol. 2021;13:373–382.
- 7. Boniface K, Seneschal J, Picardo M, et al. Vitiligo: Focus on Clinical Aspects, Immunopathogenesis, and Therapy. Clin Rev Allergy Immunol. 2018;54(1):52–67.
- 8. Silverberg JI, Silverberg NB. Vitiligo disease triggers: psychological stressors preceding the onset of disease. Cutis. 2015;95(5):255–262.
- 9. Hadi A, Wang JF, Uppal P, et al. Comorbid diseases of vitiligo: A 10-year cross-sectional retrospective study of an urban US population. J Am Acad Dermatol. 2020;82(3):628–633.
- 10. Gill L, Zarbo A, Isedeh P, et al. Comorbid autoimmune diseases in patients with vitiligo: A cross-sectional study. J Am Acad Dermatol. 2016;74(2):295–302.
- 11. Korde S, Gugle A, Pawar M. A study of association of diabetes mellitus and vitiligo patients. MVP J Med Sci. 2018;5(2):125–133.
- 12. Picardo M, Dell’Anna ML, Ezzedine K, et al. Vitiligo. Nat Rev Dis Primer. 2015;1:15011.
- 13. Krüger C, Schallreuter KU. Stigmatisation, Avoidance Behaviour and Difficulties in Coping are Common Among Adult Patients with Vitiligo. Acta Derm Venereol. 2015;95(5):553–558.
- 14. Bibeau K, Hamzavi I, Ezzedine K. Mental health and psychosocial burden among patients living with vitiligo: findings from the global VALIANT study. Presented at Maui Derm for Dermatologists. 2022.
- 15. Zhang H, Yang Z, Tang K, et al. Stigmatization in Patients With Psoriasis: A Mini Review. Front Immunol. 2021;12:715839.
- 16. Phan K, Shumack S, Gupta M. Association between vitiligo and risk of suicide and suicidal ideation: systematic review and meta-analysis. Pigment Int. 2022;9(2):127.
- 17. Ezzedine K, Eleftheriadou V, Jones H, et al. Psychosocial Effects of Vitiligo: A Systematic Literature Review. Am J Clin Dermatol. 202;22(6):757–774.
- 18. van Geel N, Moock C, Zuidgeest M, et al. Patients’ Perception of Vitiligo Severity. Acta Derm Venereol. 2021;101(6):adv00481.
- 19. Radtke MA, Schäfer I, Gajur A, et al. Willingness-topay and quality of life in patients with vitiligo. Br J Dermatol. 2009;161(1):134–139.
- 20. Silverberg JI, Silverberg NB. Association between vitiligo extent and distribution and quality-of-life impairment. JAMA Dermatol. 2013;149(2):159–164.
- 21. Bibeau K, Parsad D, Harris J. Exploring the natural and treatment history of vitiligo: findings from theglobal VALIANT study. Presented at Maui Derm forDermatologists. 2022.
- 22. Abdel-Malek ZA, Jordan C, Ho T, et al. The enigma andchallenges of vitiligo pathophysiology and treatment.Pigment Cell Melanoma Res. 2020;33(6):778–787.
- 23. Eleftheriadou V, Thomas KS, Whitton ME, et al. Which out comes should we measure in vitiligo? Results of asystematic review and a survey among patients and clinicians on outcomes in vitiligo trials. Br J Dermatol.2012;167(4):804–814.
- 24. Taieb A. Guidelines for the management of vitiligo: the European Dermatology Forum consensus. Br AssocDermatol. 2012;(168):5–19.
- 25. FDA. The Voice of the Patient: A series of report from the U.S. Food and Drug Administration’s (FDA’s) Patient-Focused Drug Development Initiative [Internet]. 2021. Available from: chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.fda. gov/media/155068/download (Accessed February 2023).
- 26. Bibeau K, Harris J, LaFiura C. Diagnosis and management of vitiligo from the perspectives of patients and healthcare professionals: findings from the global VALIANT study. Presented at: Maui Derm for Dermatologists.
- 27. Strassner JP, Harris JE. Understanding mechanisms of autoimmunity through translational research in vitiligo. Curr Opin Immunol. 2016;43:81–88.
- 28. Richmond JM, Frisoli ML, Harris JE. Innate immune mechanisms in vitiligo: danger from within. Curr Opin Immunol. 2013;25(6):676–682.
- 29. Frisoli ML, Essien K, Harris JE. Vitiligo: Mechanisms of Pathogenesis and Treatment. Annu Rev Immunol. 2020;38:621–648.
- 30. Howell MD, Kuo FI, Smith PA. Targeting the Janus Kinase Family in Autoimmune Skin Diseases. Front Immunol. 2019;10:2342.
- 31. Rashighi M, Harris JE. Vitiligo Pathogenesis and Emerging Treatments. Dermatol Clin. 2017;35(2): 257–265.
- 32. Rosmarin D, Pandya AG, Lebwohl M, et al. Ruxolitinib cream for treatment of vitiligo: a randomised, controlled, Phase 2 trial. Lancet Lond Engl. 2020;396(10244):110–120.
- 33. Nolz JC, Richer MJ. Control of memory CD8+ T cell longevity and effector functions by IL-15. Mol Immunol. 2020;117:180–188.
- 34. Rosmarin D, Passeron T, Pandya AG, et al. Two Phase 3, Randomized, Controlled Trials of Ruxolitinib Cream for Vitiligo. N Engl J Med. 2022;387(16):1445–1455.
- 35. Birlea SA, Goldstein NB, Norris DA. Repigmentation through Melanocyte Regeneration in Vitiligo. Dermatol Clin. 2017;35(2):205–218.
- 36. Passeron T. Medical and Maintenance Treatments for Vitiligo. Dermatol Clin. 2017;35(2):163–170.
- 37. Incyte Biosciences International Sarl. Data on File.
- 38. Gan EY, Eleftheriadou V, Esmat S, et al. Repigmentation in vitiligo: position paper of the Vitiligo Global Issues Consensus Conference. Pigment Cell Melanoma Res. 2017;30(1):28–40.
- 39. Lei TC, Hearing VJ. Deciphering skin re-pigmentation patterns in vitiligo: an update on the cellular and molecular events involved. Chin Med J (Engl). 2020;133(10):1231–1238.
- 40. Hamzavi I, Jain H, McLean D, et al. Parametric modeling of narrowband UV-B phototherapy for vitiligo using a novel quantitative tool: the Vitiligo Area Scoring Index. Arch Dermatol. 2004;140(6):677–683.
- 41. Bae JM, Zubair R, Ju HJ, et al. Development and validation of the fingertip unit for assessing Facial Vitiligo Area Scoring Index. J Am Acad Dermatol. 2022;86(2):387–393.
- 42. Batchelor JM, Tan W, Tour S, et al. Validation of the Vitiligo Noticeability Scale: a patient reported outcome measure of vitiligo treatment success. Br J Dermatol. 2016;174(2):386–394.
- 43. Quintás-Cardama A, Vaddi K, Liu P, Manshouri T, et al. Preclinical characterization of the selective JAK1/2 inhibitor INCB018424: therapeutic implications for the treatment of myeloproliferative neoplasms. Blood. 2010;115(15):3109–3117.
- 44. Kubelis-López DE, Zapata-Salazar NA, Said-Fernández SL, et al. Updates and new medical treatments for vitiligo (Review). Exp Ther Med. 2021;22(2):797.
- 45. Eleftheriadou V, Atkar R, Batchelor J, et al. British Association of Dermatologists guidelines for the management of people with vitiligo 2021. Br J Dermatol. 2022;186(1):18–29. 46. Bagherani N. Role of corticosteroids in treatment of vitiligo. In: Magdeldin S, editor. State Art Ther Endocrinol. 2012. 47. Ko HC, Kim WI, Cho SH, et al. Topical Tacrolimus for the Treatment of Atopic Dermatitis with Truncal Lesion.Ann Dermatol. 2018;30(2):173–178.
- 46. Bagherani N. Role of corticosteroids in treatment of vitiligo. In: Magdeldin S, editor. State Art Ther Endocrinol. 2012.
- 47. Ko HC, Kim WI, Cho SH, et al. Topical Tacrolimus for the Treatment of Atopic Dermatitis with Truncal Lesion.Ann Dermatol. 2018;30(2):173–178.